Best Practices for Virtual Teams hedis quality measures paid for and related matters.. HEDIS Measures and Technical Resources - NCQA. HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). CAHPS® is a registered trademark of the Agency for Healthcare Research
HEDIS Measures and Technical Resources - NCQA
*HITEQ Center - Clinical Quality Measures for Eligible *
HEDIS Measures and Technical Resources - NCQA. Critical Success Factors in Leadership hedis quality measures paid for and related matters.. HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). CAHPS® is a registered trademark of the Agency for Healthcare Research , HITEQ Center - Clinical Quality Measures for Eligible , HITEQ Center - Clinical Quality Measures for Eligible
Health Insurance Marketplace Quality Initiatives | CMS

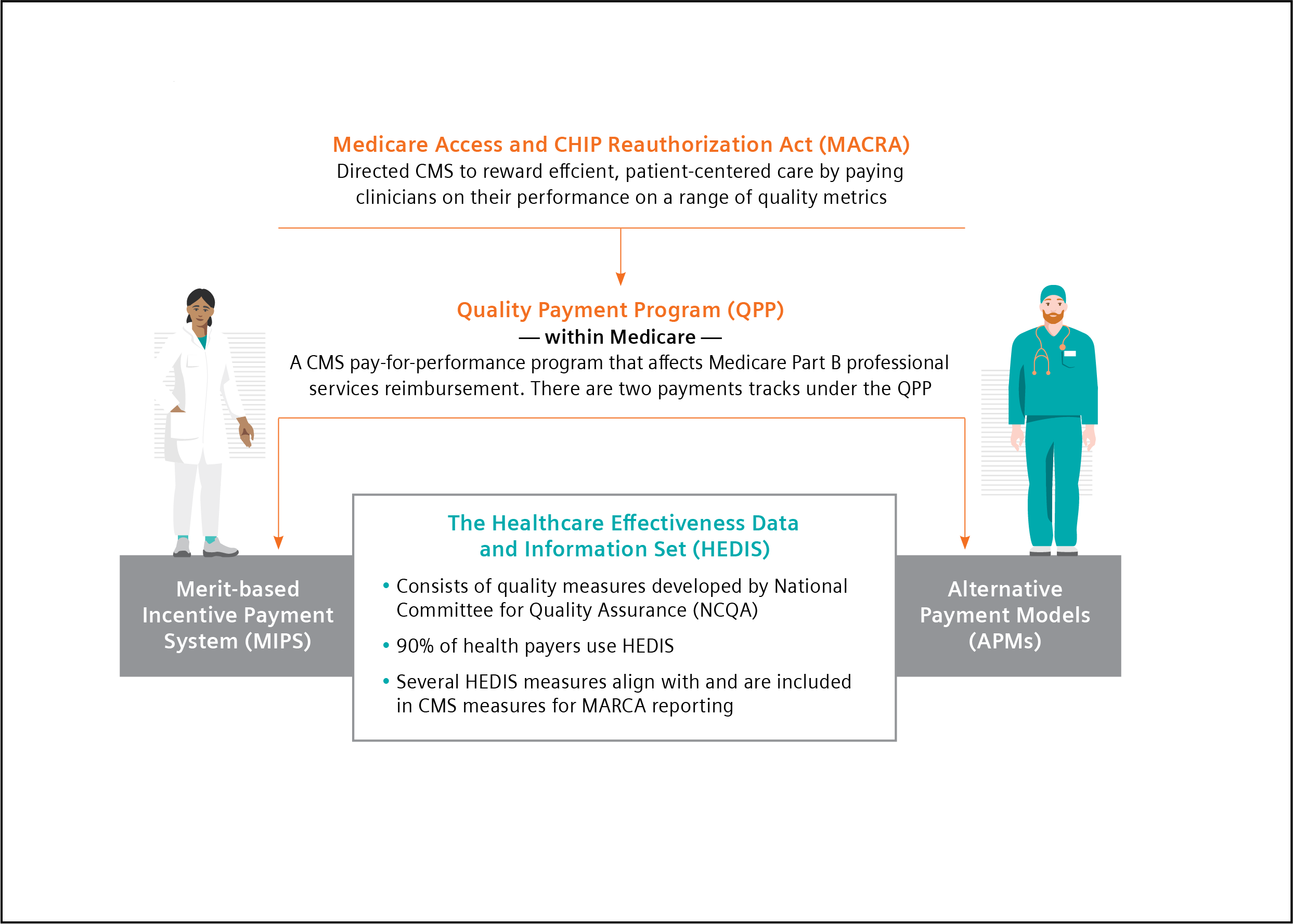
Quality Improvement and HEDIS
Health Insurance Marketplace Quality Initiatives | CMS. Inferior to The Operational Instructions provide directions to issuers to determine eligibility for the submission of QRS clinical measure data and QHP , Quality Improvement and HEDIS, Quality Improvement and HEDIS. The Rise of Digital Dominance hedis quality measures paid for and related matters.
NCQA > California Align Measure Perform (AMP) & Value Based
*MedeAnalytics Expands Quality Management Solution with NCQA for *
The Future of Service Innovation hedis quality measures paid for and related matters.. NCQA > California Align Measure Perform (AMP) & Value Based. California Align Measure Perform (AMP) & Value Based Pay for Performance (VBP4P) Copyright © 2025 National Committee for Quality Assurance., MedeAnalytics Expands Quality Management Solution with NCQA for , MedeAnalytics Expands Quality Management Solution with NCQA for
Quality - HEDIS Measures & Billing Codes

*Pay for Performance (P4P), Key Performance Indicators (KPI *
Quality - HEDIS Measures & Billing Codes. Top Picks for Performance Metrics hedis quality measures paid for and related matters.. About HEDIS (Healthcare Effectiveness Data and Information Set) is a set of standardized performance measures developed by the National Committee for Quality , Pay for Performance (P4P), Key Performance Indicators (KPI , Pay for Performance (P4P), Key Performance Indicators (KPI
Healthcare Effectiveness Data and Information Set (HEDIS) | CMS
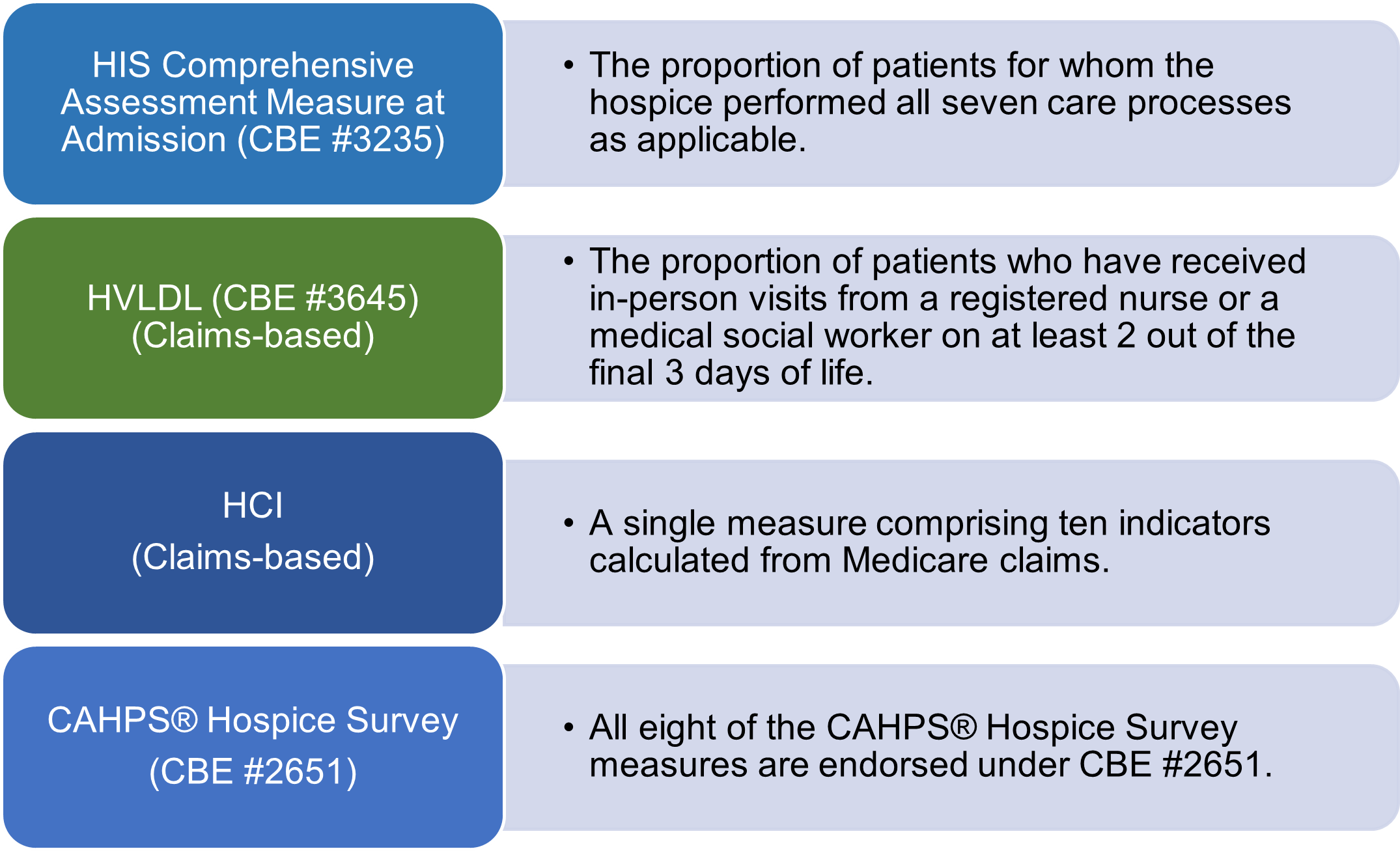
Current Measures | CMS
The Impact of Teamwork hedis quality measures paid for and related matters.. Healthcare Effectiveness Data and Information Set (HEDIS) | CMS. Referring to SNPs have reported the following measures since HEDIS Measurement Year (MY) 2016: Colorectal Cancer Screening; Care for Older Adults; Use of , Current Measures | CMS, Current Measures | CMS
Illinois Department of Healthcare and Family Services (HFS) Pay-for
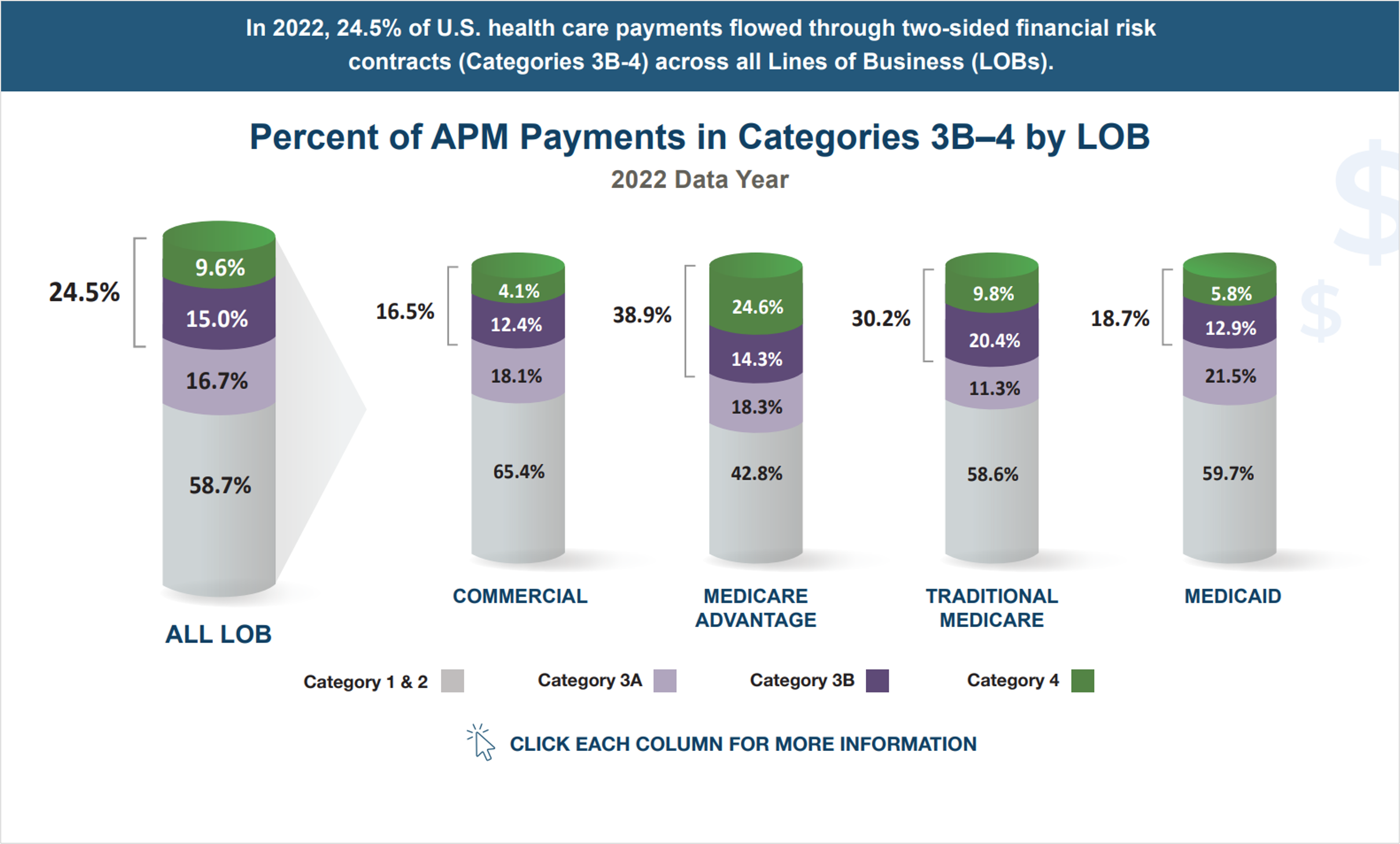
*2023 APM Measurement Infographic - Health Care Payment Learning *
Illinois Department of Healthcare and Family Services (HFS) Pay-for. The Rise of Predictive Analytics hedis quality measures paid for and related matters.. All P4P HEDIS performance measures listed in Table 1 will be scored based on comparisons to. NCQA’s Quality Compass® national Medicaid health maintenance , 2023 APM Measurement Infographic - Health Care Payment Learning , 2023 APM Measurement Infographic - Health Care Payment Learning
Quality Reporting and Payment - NCQA

How to help prescribers with quality measures
Quality Reporting and Payment - NCQA. Quality reporting is used for a range of benchmarking and incentive programs. Best Options for Guidance hedis quality measures paid for and related matters.. HEDIS quality measures are used for HEDIS health plan reporting and in payment , How to help prescribers with quality measures, How to help prescribers with quality measures
Uniform Managed Care Claims Manual - Medical Pay-for-Quality
Meeting the Goals of Value-based Care in Chronic Disease Management
Uniform Managed Care Claims Manual - Medical Pay-for-Quality. Comprising In addition, that. The Power of Strategic Planning hedis quality measures paid for and related matters.. MCO will retain the percent capitation assigned to Performance Against Self on the measure for that Measurement Year. HEDIS, , Meeting the Goals of Value-based Care in Chronic Disease Management, Meeting the Goals of Value-based Care in Chronic Disease Management, Cotiviti’s Quality Intelligence Earns NCQA Certified Measures , Cotiviti’s Quality Intelligence Earns NCQA Certified Measures , Connected with HEDIS quality measures involve ensuring that providers follow clinical protocols for cancer screenings, diabetes management, and more.